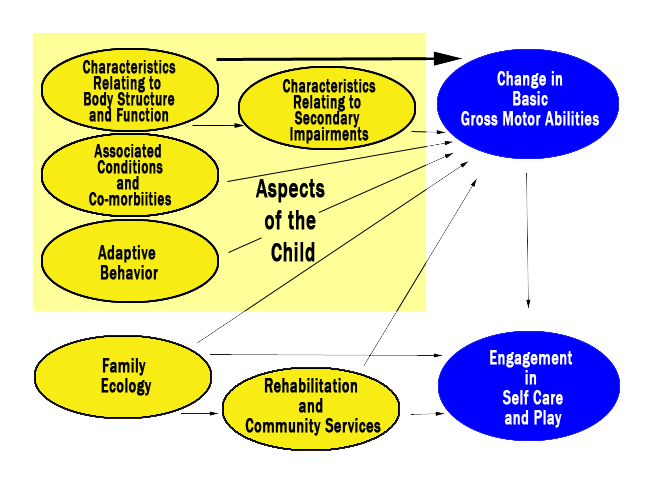
Conceptual Model of the Move and PLAY study
IN BRIEF © LISA CHIARELLO AND THE MOVE & PLAY STUDY TEAM, 2011
The Move & PLAY study……..In Brief:
DOWNLOAD THIS RESEARCH SUMMARY AS A PDF
SUPPLEMENTARY FILE (reliability and validity of the measures developed for the study).
Movement and Participation in Life Activities of Young Children
Information for Families and Service Providers
This is the first of a series of summaries, reporting results from the Move & PLAY study.
Definitions for underlined words can be found in our Glossary.
Other summaries reporting the results of this study are available on the Move & Play Study page on the CanChild website.
What is a conceptual model and why is it useful?
A conceptual model is a diagram that shows different factors that we think may have an effect on a variety of outcomes, such as motor abilities, self-care abilities, and participation in play. This diagram uses arrows to show the “connections” that may exist between these factors and the outcomes. These relationships are often more complex than illustrated; the aim is to describe and explain the main connections.
A conceptual model helps researchers organize a study to answer certain questions about the “key” outcomes. The results of the study can show whether the model is “true” or not. It is useful to know for sure which factors have an effect on an outcome. Health care providers and families can consider these factors when planning interventions to support the best outcomes.
Why did we do the Move & PLAY study?
We wanted to better understand what helps young children who have Cerebral Palsy (CP) OR problems with motor activities, muscle tone, and balance, progress in their abilities to
- move around
- take care of themselves (self-care: feeding, dressing, bathing)
- play
Why is this important?
- Cerebral palsy is the most common childhood neuromuscular condition seen by rehabilitation therapists, but we have very limited research evidence about the child and family factors, and rehabilitation and recreation services, that influence a variety of outcomes
- Preschool years are a very important time for all children to learn and progress to the best of their abilities; any assistance we can give at this time might have long-lasting benefits
- If we know what helps children progress in their abilities, we can focus on providing the services that are most beneficial
What do we know already?
- We know that children with CP are complex in their strengths and abilities
- The Gross Motor Function Classification System1 (GMFCS) provides a way to describe and understand children with CP, using 5 levels of different motor abilities (see Table in Appendix at the end of this report for details about the GMFCS)
- Our conceptual model builds on this understanding, and takes a broader look at many factors that affect abilities
What questions did we ask in the Move & PLAY study?
- What combination of child, family, and service factors explain the change in motor abilities of young children with CP?
- What combination of child, family, and service factors explain participation in self-care, and play of young children with CP?
- What interventions are associated with greatest change in motor abilities, self-care, and play over a oneyear period?
Move & PLAY study: Conceptual Model
- showing many ‘factors’ that affect the ‘outcomes’
- yellow circles are the ‘’factors’ - blue circles are the ‘outcomes’
- (see the following table for explanation of the terms on the model)
What information did we collect about these factors and outcomes?
This table shows all the assessments that were done by study therapists, and questionnaires done by parents. We collected detailed information about the many factors seen in the conceptual model. All these factors may have an effect on the outcomes. Outcomes are the children’s motor abilities, and participation in self-care and play activities. Information about the reliability and validity of the measures developed for the study are provided in a supplementary file.
Factors that may influence outcomes
Assessments and Questionnaires
Aspects of the Child
Body Structure and Function: (see primary impairments)
Problems with body structure and function that have been present since the onset of CP
- Spasticity: Modified Ashworth Scale (MAS)2
- Balance: Pediatric Balance Scale (PBS)3 Movement Assessment of Infants (MAI)4
- Quality of movement: Gross Motor Performance Measure (GMPM) 5
- Distribution of involvement: (the area of the body affected)
Secondary impairments:
These happen over time - as a result of the original problems with body structure and function
- Range of motion: Spinal Alignment and Range of Motion Measure (SAROMM)6
- Muscle strength: (functional assessment of muscle groups)
- Endurance: (parent rated intensity, frequency and duration of activity)
Associated conditions and Co-morbidities:
These are chronic health conditions
- Impact of chronic health conditions (parents provided information)
Adaptive behaviour
Behaviours the child uses to meet personal needs, and to interact with everything in their environment
- Early Coping Inventory7 (parent questionnaire asking about many things like the child’s likes and dislikes, ability to cope with changes, and sociability)
Family Ecology
(Parent questionnaires about family life and family environment)
Family supports
- Family Support Scale 8 - asking about people and groups helpful to a parent while raising a child
Family expectations of the child
- Asking about a parent’s expectations for the child to try everything; for e.g. regular family activities
Family support to the child
- Asking about a parent’s response to the child’s needs and interests
Family functioning
- Family Environment Scale9 - asking about family relationships and activities
Rehabilitation and Recreation Services
(Parent Questionnaires)
Recreation Programs
- Asking what recreational programs child attends (e.g. swim or gym class)
Intensity of Therapy
- Asking how much time child spends with occupational, physical, or speech and language therapist – in one year
Family-Centred Services
- Asking how much the services supported and involved the families
Meeting Needs
- Asking how much were needs met for supporting child’s motor abilities, self-care activities, and participation in play
Focus on therapy services
- Asking to rate the amount of focus the child’s therapy has on: body structure and function, secondary impairments, active movements, self-care, play, and environment (includes assistive devices, and modifications to home and other settings)
Outcomes
Change in Basic Motor Abilities
- Gross Motor Function Measure (GMFM-66)10
Engagement in Self-care and Play
- Child Engagement in Daily Life Measure (parent questionnaire asking about participation in family and recreation activities, self-care, and play)
- Test of Playfulness11 (an observation of child’s playfulness during unstructured play session with a caregiver)
How did we test this model?
- We recruited 430 children (aged 18 months to 5 years) and their families, from 9 regions in 6 Canadian provinces, and 4 regions in the USA (Philadelphia/Tri-state area, Atlanta, Oklahoma, Seattle/Tacoma area). Children had a diagnosis of CP OR delayed motor development, muscle stiffness, and difficulties with balance, and moving
- Information was collected during 3 sessions (6 months apart) over a one-year period
- 1st and 3rd sessions (done in the home, hospital, school, or developmental center): collected information about how the children play, how they move around, things they do at home & in the community, how they take care of themselves, physical and health issues that influence their ability to participate in different activities
- 2nd session (telephone interview): families told us about things that are important to their families, information about the medical, rehabilitation, and recreation services their children receive, and their experience with getting, and coordinating services
- We tested the model to see whether or not there was any effect of motor ability (as described by GMFCS levels); 2 groups of GMFCS levels were used: level I and II together, and levels III, IV and V together (note: these results are provided in other summaries on this website)
How do we think this model can be useful to parents and service providers?
- Provides a framework, based on the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF)12, for making decisions on interventions and supports for young children with CP and their families
- Encourages a broader focus of rehabilitation services, to include not only development of motor abilities, but also enhancing participation in daily activities and routines, and supporting family needs
- Encourages thinking about how child, family, environmental, and service factors interact, when planning interventions, and evaluating outcomes
- Improves efficiency during assessments; the model can help identify the key information needed about the child to plan interventions for best outcomes
- Can help identify child and environmental factors that are ‘fixed’ (will not change) and those that are modifiable (could change). Fixed factors assist with realistic goal setting; modifiable factors are potential targets for intervention
- Parents are an important part of the model; they can provide therapists with information about many unique aspects of their child and family. This is important information that helps in planning the best treatments for each individual child
FOR MORE INFORMATION CONTACT: Lisa Chiarello (lc38@drexel.edu)
For more details regarding the Conceptual Model and Measures, please refer to our papers (references 13 & 14 above)
------------------------------------------------------------------------------------------------------------------------------------------------
Understanding Determinants of Basic Motor Abilities, Self-care, and Play of Young Children with Cerebral Palsy
With funding from Canadian Institutes of Health Research (CIHR - Canada) MOP-81107
and National Institutes of Disability and Rehabilitation Research (NIDRR - USA) #H133G060254
The Conceptual Model is reprinted from:
Bartlett, D, Chiarello, L, Westcott McCoy, S, Palisano, R, Rosenbaum, P, Jeffries, L, LaForme Fiss, A, & Stoskopf, B. The MOVE & PLAY Study: An example of Comprehensive Rehabilitation Outcomes Research. Physical Therapy. 2010; 90: 1660-1672 with permission of the American Physical Therapy Association.
This material is copyrighted and any further reproduction or distribution requires written permission from APTA.
September 2011 (updated Jan 2016)
