Recreation and Rehabilitation Services - Move & Play
Information for Families and Service Providers
Who participated?
430 preschool (age 18 months to 5 years) children with Cerebral Palsy (CP) and their families were recruited from many regions of Canada and the USA; all children had CP or problems with motor activities, muscle tone, and balance.
What did we do?
We focused on learning what helps children with CP progress in their ability to move around, take care of themselves (self-care: feeding, dressing, bathing), and play.
What was our goal?
We wanted to find out what we can change about the way we help young children who need rehabilitation services, so we can focus on providing the services that are most beneficial.
How did we do this?
We collected information about many characteristics of the child, the family, and the recreation and rehabilitation services they receive, during 3 sessions over a one-year period.
Looking at Recreation and Rehabilitation Services
This report focuses on what parents told us about the recreation and rehabilitation services their children received. We collected information about various aspects of these services at the 2nd session, using a parent questionnaire developed by the research team.
Services questionnaire: 5 part questionnaire asking about:
- Types and frequency of programs and services such as: recreational programs; early intervention and school programs; physical, occupational, and speech therapy; medical services (doctors, clinics, homecare)
- Availability and accessibility of programs and services
- Coordination of programs and services
- Extent to which these programs and services met the children’s and families’ needs
- Focus (content) of therapy services (e.g. focus on balance or stretching)
We also asked about: aspects of family-centred care, such as: degree of information sharing between families and therapist; quality of relationship with therapist; and families’ abilities to integrate therapy recommendations into daily routine.
Information about the reliability and validity of this measure is provided in a supplementary file.
Why is it important to know about Recreation and Rehabilitation Services?
- Little is known about which aspects of service influence activities of daily life of young children with CP. What is the best service delivery method and frequency of services? This remains unclear
- Family-centred care is a hallmark in pediatric rehabilitation and therapists have reported challenges in implementing this. It is important to understand parents’ perspectives on the extent to which services are: accessible, coordinated, collaborative, comprehensive, and responsive to children’s and families’ needs
- Currently, there is a shift away from interventions focused on impairments, and movement towards interventions that focus on activity and participation. However, therapists need more information about what services are most relevant to enhance activity and participation
Please note, there is another summary regarding Services: “A closer look at recreation and rehabilitation services”.
What did we learn?
Please keep in mind that these results are based on averages for the total group. Children are individuals and not all would fit the results described below.
We looked at the effect of children’s gender, age, and motor ability on various aspects of services received. Motor ability was measured by the Gross Motor Functional Classification System1 (GMFCS). GMFCS has 5 levels of motor abilities; children in level I have the highest motor abilities, and children in level V the least motor abilities.
Parent respondents
The majority (92%) of parents who participated were mothers.
Influence of Gender
There was no difference between boys and girls in any aspect of the recreation and rehabilitation services they received.
Participation in Recreation Programs:
Leisure and recreational activities included swimming, gym programs, horseback riding, dance and movement classes, sports, and other programs such as music classes.
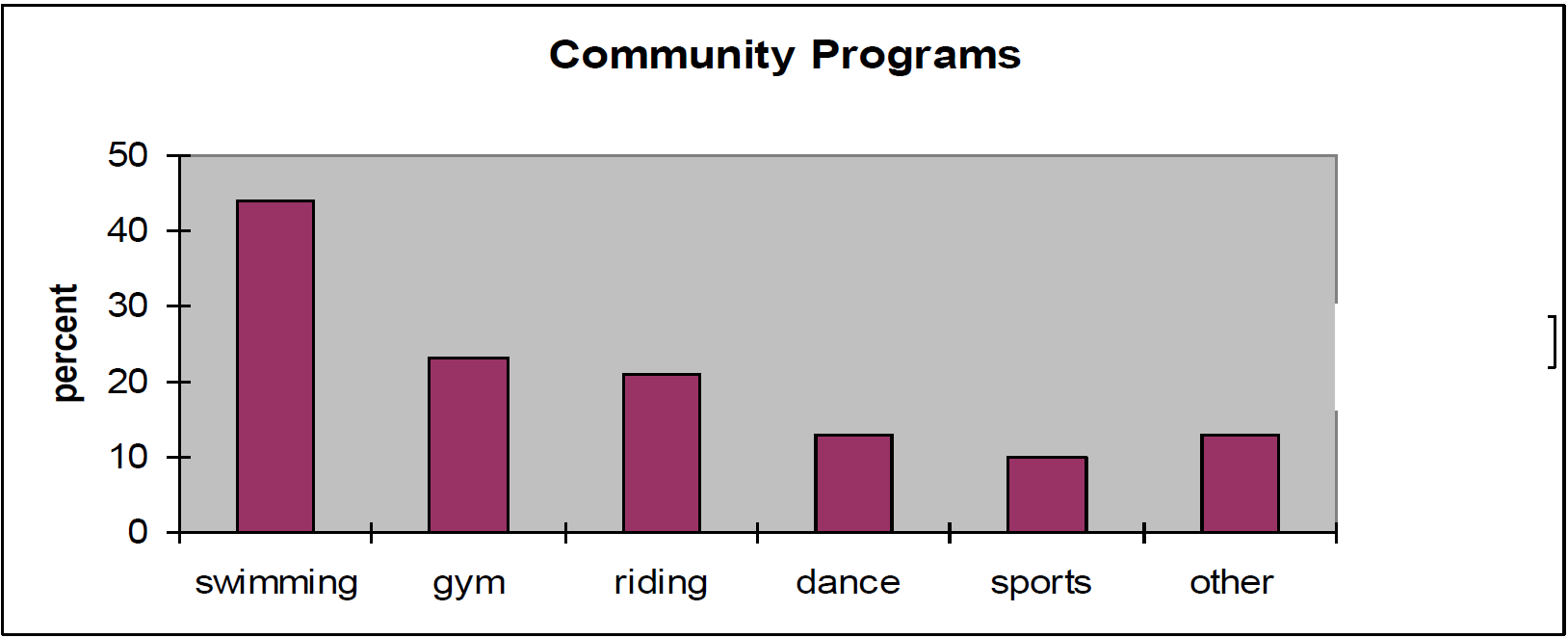
- On average, children participated in 1 recreation program
- Half of the children participated in 1 or 2 programs
- 36% of children did not participate in any recreation programs
- Older children (over 30 months) participated in more programs than younger children (18 – 30 months)
- Participation in recreation programs was similar for children of all motor abilities
Types and Frequency of Rehabilitation Services
We asked about services received from physical, occupational or speech therapists, at any location. Children received services at early intervention programs, schools, hospital or private clinics, and rehabilitation centers. The total time was calculated for each child by adding up all time spent in therapy at any of these locations.
- Age of the child made no difference in the amount of therapy received
Physical Therapy (PT) services:
- 94% of children received PT; average amount of PT was 4.5 hours per month
- GMFCS level had a significant effect: children with higher motor abilities (level I) had statistically significant less PT time than all others. Children in levels II to V had a similar amount of PT ranging from 5.2 to 5.7 hours per month, compared to children in level I who had an average of 3 hours per month
Occupational Therapy (OT) services:
- 85% of children received OT; average amount of OT was 3.2 hours per month
- GMFCS level had a significant effect: children with higher motor ability received less hours of OT; but the difference was significant only for children in level I compared to those in level V (2.6 hours /month vs. 4.1 hours)
Speech Therapy services:
- 74% of children received speech therapy; average amount was 2.7 hours per month
- GMFCS level had a significant effect: children with higher motor abilities (level I) had significantly less speech therapy than those children in level V. The amount of speech therapy varied from 2.1 hours for children in level I, to 3.8 hours for children in level V
Coordination of Services:
- Parents were asked to rate how well various service providers worked together, and with the family (service providers included doctors, nurses, therapists, early intervention workers, and teachers)
- Scores were on a scale of 1-5: 1= not at all (did not work well together) and 5= excellent
- Average score was 4.3; this means that parents rated coordination a little better than “good “
- Age and motor ability of children did not make any difference in scores
Services Meeting Needs
- Parents were asked to rate how well the services they received met the needs of their children in supporting development of motor abilities, self care abilities, and participation in play
- Scores were on a scale of 1-5: 1=not at all, and 5=completely
- Average score was 3.8 which is close to saying that needs were met “to a great extent”
- Age of children did not make any difference in scores
- GMFCS level had a significant effect, but differences were small. In general, children with higher motor abilities (level I) had needs met “to a great extent”, while children in level V had needs met to a “moderate extent”
Focus of Therapy Services
Scores were on a scale of 1-5 (1=not at all; 5=a very great extent) higher scores mean greater focus
Parents rated how much the child’s therapy focused on:
- Primary Impairments (balance, distribution of involvement, quality of movement, spasticity)
- Secondary Impairments (muscle strength, range of motion, endurance)
- Environment (assistive devices, modifications to home, equipment)
- Family-centeredness
- Activity (related to mobility, transferring, tasks involving movement)
- Self Care routines
- Structured play activities
Average scores are shown below for each focus of therapy:
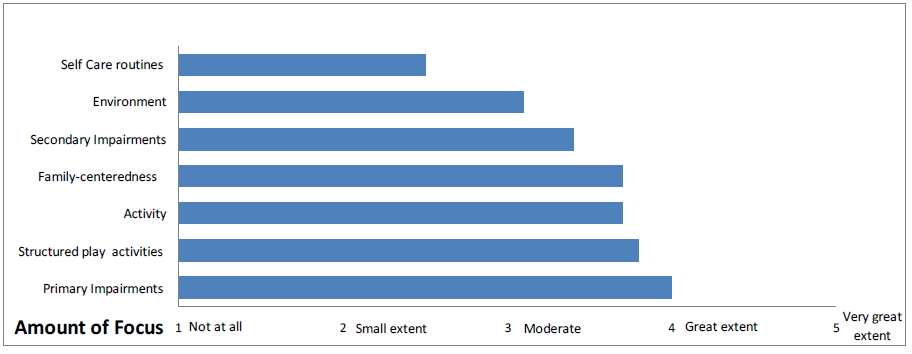
- Parents also rated their ability to include therapy recommendations into daily routines; average rating was “4” which means they did this “to a great extent”
- Children’s age did not make a difference except for “focus on self care” and “focus on secondary impairments. Parents of older children reported a greater focus of therapy on self-care routines and secondary impairments
- GMFCS level had a significant effect for some types of focus. Children with lower motor abilities (level V) had less focus on “activity”, than all other children. Children with higher motor abilities (leveI I) had less focus on “environmental modifications” than all other children. Children in level I had greater focus on “self care routines” than children in level V
What does this mean?
Thoughts for families
- Partner with service providers to advocate for recreation programs in your community
- Parents who want recreational programs for their children can ask their therapist about options in their community and help to locate and connect with programs
- Parents should expect that team members will communicate with them and with other service providers about the services the family receives
- Parents should expect to receive services that meet their children’s needs in supporting development of motor and self care abilities, and play
- Parents are encouraged to discuss with therapists the focus of therapy services, to make sure that services are meeting their priorities for their children
Thoughts for service providers
- Collaborate with families, agencies, and other service providers, such as recreational therapists, to develop a range of community programs
- Ask families how much they and their children participate in recreational programs, and if they are interested in receiving help to locate or connect with the options available in their community
- Therapists are encouraged to communicate and partner with other services providers, and the family, to ensure coordinated services are provided
- It is important for therapists to be accountable for their services and to evaluate how well they are meeting the needs of families and children
- On average, parents’ report of focus on the ‘environment’ and ‘self care routines’ was lower than for all other areas of focus; perhaps this shows a need for a greater focus on maximizing adaptations to the environment and assisting with self care tasks
This is the fourth of a series of summaries, reporting results from the Move & PLAY study.
Other summaries reporting the results of this study are available on the Move & Play Study page on the CanChild website.
References:
1. Palisano RJ, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B: Development and validation of a Gross Motor Function Classification System for children with cerebral palsy. Developmental Medicine and Child Neurology 39:214-223, 1997.
For more details regarding Services, please refer to our paper: - Palisano R, Begnoche D, Chiarello L, Bartlett D, McCoy S, Chang H-J. Amount and Focus of Physical Therapy and Occupational Therapy for Young Children with Cerebral Palsy. Physical and Occupational Therapy in Pediatrics. 2012; 32(4): 368-382.
FOR MORE INFORMATION, CONTACT: Lisa Chiarello (lc38@drexel.edu)
------------------------------------------------------------------------------------------------------------------------------------------------
Understanding Determinants of Basic Motor Abilities, Self-care, and Play of Young Children with Cerebral Palsy
With funding from Canadian Institutes of Health Research (CIHR - Canada) MOP-81107
and National Institutes of Disability and Rehabilitation Research (NIDRR - USA) #H133G060254
December 2012 (Updated Jan 2016)
